Link to the original article
PDF version of the article
Redlining of Decades Past Associated With Heart Disease Today
Despite being banned, redlining continues to affect communities
Published July 5, 2022
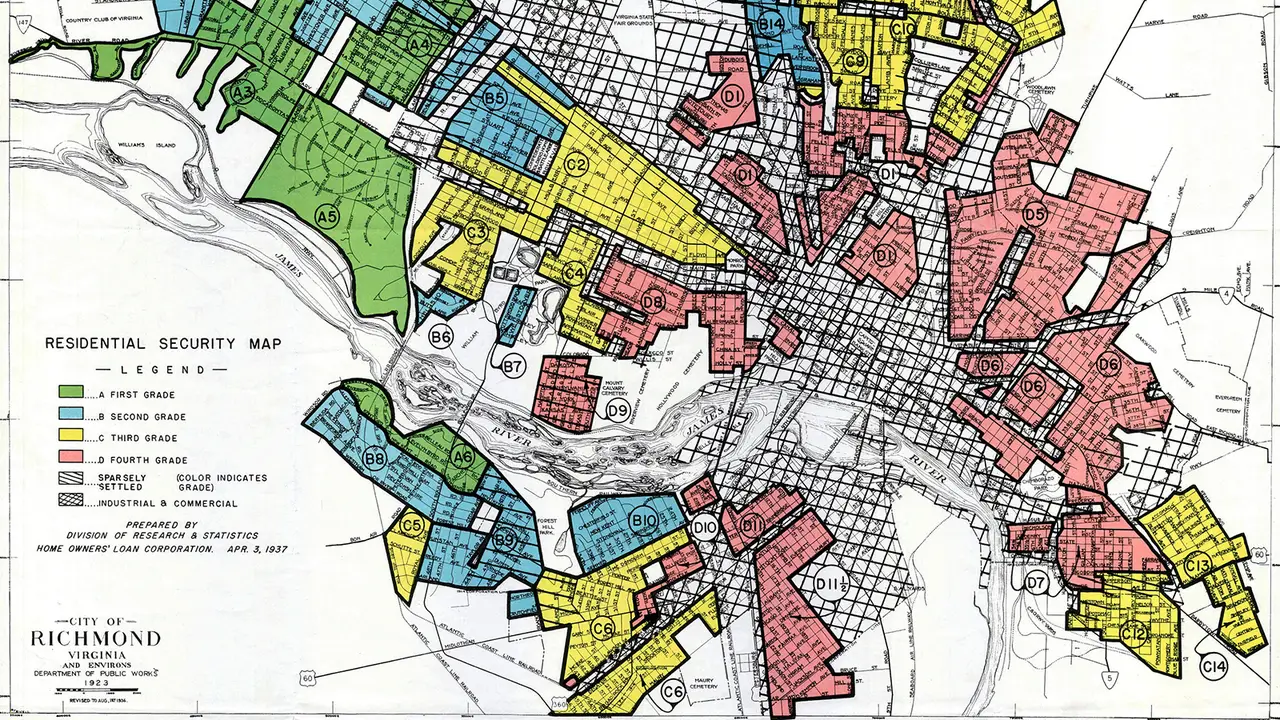
More than 60 years after redlining was banned, the historical discriminatory housing practice was still associated with cardiovascular disease and its risk factors in a cross-sectional study.
Compared with the most desirable ("A grade") communities as judged by the federal Home Owners' Loan Corporation (HOLC) in the 1930s, neighborhoods deemed more undesirable tended to have less cholesterol screening and fewer routine health visits, but a higher prevalence of diabetes, obesity, hypertension, and smoking as recently as 2021.
In the modern era, historically redlined (or HOLC "D grade") areas were also associated with a higher prevalence of coronary artery disease (CAD), stroke, and chronic kidney disease, Sadeer Al-Kindi, MD, of Case Western Reserve University School of Medicine in Cleveland, Ohio, and colleagues reported in the Journal of the American College of Cardiology.
"We already know historic redlining has been linked with modern-day health inequities in major urban areas, including asthma, certain types of cancer, preterm birth, mental health, and other chronic diseases," Al-Kindi said in a press release.
"While ours is the first study to examine the national relationship between redlined neighborhoods and cardiovascular diseases, it's logical that many of the socioeconomic, environmental, and social impacts of redlining on other areas of residents' health outcomes would also be seen in heart disease," he continued.
Al-Kindi's group argued that although redlining was outlawed many years ago, it is still visible as geographic disparities today.
"Historically redlined neighborhoods are situated next to major sources of environmental pollution, making inhabitants more likely to experience detrimental health effects resulting from disproportionately higher exposures to ambient air pollution, less green space, and environmental toxicants such as phthalate and phenols," the authors wrote.
"Financial strain, dismantled communities, and racial discrimination experienced by many residents of redlined neighborhoods may lead to increased stress and associated adverse health outcomes," they continued.
Their study showed that people who live in redlined neighborhoods, especially minorities, were less likely to have access to health insurance, public transportation, and healthy food. These factors may contribute to worsened health outcomes and increased risk.
For the study, the researchers pooled redlining records from HOLC, contemporary neighborhood data from the 2020 U.S. Census, and health data from the CDC's PLACES database.
There were over 11,000 HOLC-graded census tracts analyzed. The investigators ruled out census tracts that did not geographically overlap by at least 20%.
Over 38.5 million Americans were studied, with 7.1% of A-graded areas, 19.4% of B-graded areas, 42% of C-graded areas, and 31.5% of D-graded areas. The proportion of Black and Hispanic individuals increased from grade A to grade D communities.
The authors cautioned that the PLACES data had been self-reported, and that another limitation of the study was that they were unable to examine confounders like behavior and genetics. They added that the term "redlining" is not standardized across studies.
Michal Ruprecht is a reporting intern at MedPage Today, based in Michigan.
Return to clips